Open access mental health support
The case for change
In Wales, we continue to see increasing numbers of people experience mental health difficulties and we are not able to consistently provide timely access to high quality mental health care for our population. There are a number of factors contributing to this, including:
- More people seeking mental health support means more people are using services, and the demand for services is exceeding what is available.
- Experiences and outcomes for people in Wales vary considerably.
- Workforce issues such as recruitment, retention and development, remain a challenge.
- There are extremely limited funding opportunities available in the current financial climate – impacting the quality of elements such as estates and digital offers.
- Experiences and outcomes for people in Wales vary considerably.
To ensure we consistently meet the needs of our population, now and in the future, we need to transform mental health care in Wales.
In Spring 2025, Welsh Government published the Mental Health and Wellbeing Strategy 2025-35. Vision statement 4 of the strategy sets out ambitions where “there are seamless mental health services – person centred, needs led, and guided to the right support first time, without delay.”

There is a strong emphasis on open access, flexible and recovery focused mental health care in Wales, which marks a shift away from traditional tiered models of care to recovery-based system approaches. Whilst the principles are not new and there are rich evidence bases around them, national commitment to deliver this across the health system is courageous. There are clear ambitions for Wales to be the first nation to achieve same-day mental health care, based on a stepped approach.
Stepped Care 2.0
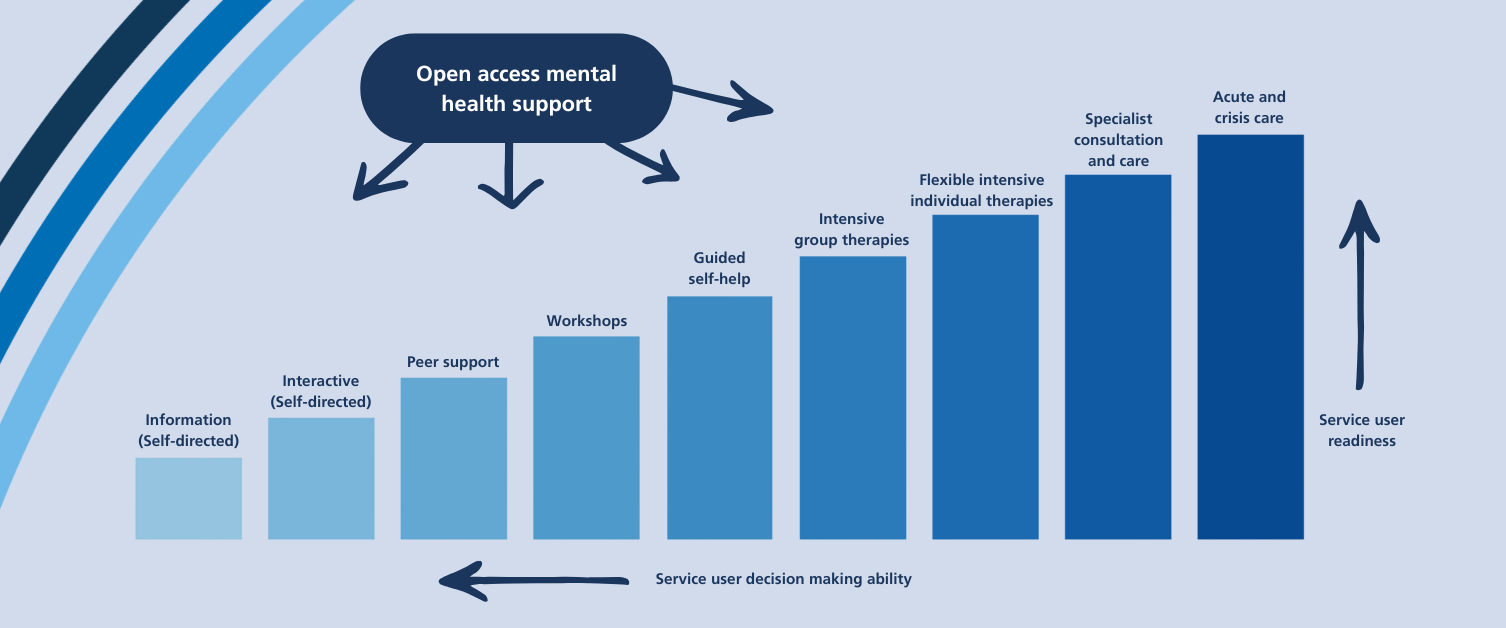
NHS Wales is adopting the Stepped Care 2.0 model to underpin transformation towards open access, flexible and recovery focused mental health care. The model, which is pioneered by Stepped Care Solutions, provides a framework for organising mental health services into a flexible system of care with open access to a range of resources and services.
The principle of open access is to get people the care they need when they need it. The approach is person-centric and focuses on the strength of individuals and communities. It recognises that there is not one approach that works for everybody, and there must be a diverse range of accessible care options based around a person’s readiness to engage and their preferences.
Guiding principles
- Social justice drives effective care systems transformation and is an intervention in itself
- Multiple and diverse care options are required as one approach will not work for everyone
- All individuals and communities have strength and capacity
- Gold standard intervention are what best fits the service user at any given time
- Professionals do not carry all the wisdom; people often know what is best for them
- Mental health literacy is required for people to make informed decisions
- An effective care system ensures people have access to care when and where it is needed
- The whole is greater than the sum of its parts; the strength of the system relies on multilevel collaboration
- Minimal interventions can produce powerful results
- There is no ideal solution; trial-and-error leads to growth and change
Core components that support experience
Whilst there are a number of components to the Stepped Care 2.0 model, there are two core components that underpin people’s experience:
Open access
People can access a variety of different services, depending on their preferences and readiness to engage. They can have same-day access to care without a referral, including one-to-one support. The approach can reduce the need for more intensive care.
One-at-a-time
The focus must be on the person’s biggest concern at that moment and should prioritise strengths and recovery. Further engagement with services is possible if the individual wants to.
Planning framework
The Stepped Care 2.0 model is organised around 9 steps that capture a range of care options that can be utilised where required, recognising one approach will not work for everyone.
People should be able to access a menu of different options, online, via phone or in person, based on their needs, preferences and readiness to engage.